We evaluated a group of 97 unvaccinated individuals (without history or current presence of symptoms of anxiety, depression and psychiatric symptoms) after a mild infection with SARS-CoV-2. We detected persistent headache, fatigue, excessive somnolence, cognitive dysfunction, and subtle microstructural white MRI abnormalities. Although the DTI analysis revealed an increase in axial diffusivity compared to controls, the investigation of the Default Mode Network with resting-state fMRI did not differ between patients and controls. In addition, the intensity of fatigue and somnolence did not correlate with the functional connectivity of the DMN.
Persistent clinical symptoms
The proportion of female responders to our online questionnaire for recruitment was higher than male responders, comparable to another study54 that conducted an online survey. There is as yet no clear evidence if sex is a risk factor for developing or perpetuating post-infectious effects of COVID-19. However, a recent meta-analysis of 134 cohorts reported that women and female cohorts were more likely to have experience deterioration of mental health55. Besides, other studies have demonstrated that female gender is associated with long COVID syndrome56 and more frequent post-infection fatigue44.
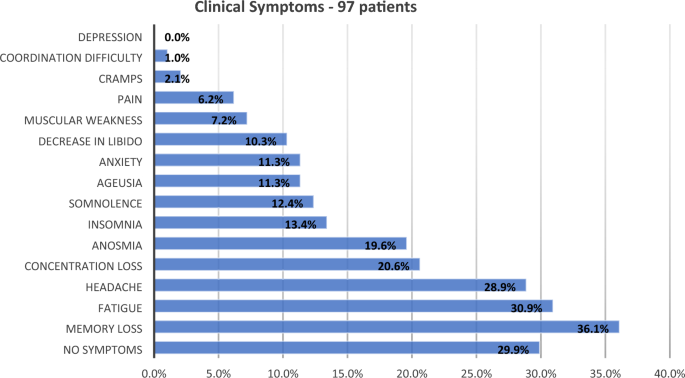
Two months after the acute period of COVID-19 infection, the most frequently reported symptoms were memory difficulties (36.1%), fatigue (30.9%), and headache (28.9%), following previous reports54,57. Our findings are in accordance with one recent study that compared 138,818 individuals with COVID-19 infection with 5,985,227 without COVID-19 after 2 years of follow-up and confirmed an increased risk of post-acute sequelae in non-hospitalized individuals, including mental health problems, neurologic dysfunction, and fatigue58. Although fatigue was self-reported by one-third of patients, the examination of CFQ-11 scores revealed a higher frequency of fatigue in patients (83.5%) compared to controls (62%), confirming that symptoms of fatigue persist regardless the severity of acute infection, as previously reported in a group of 128 individuals examined with a median interval of 10 weeks after the initial symptoms of COVID-1944. As recently reported59, we also identified excessive somnolence in the group of patients (35%), compared to the controls (11%). Overall, after excluding subjects with current (or past) symptoms of anxiety (or depression), we demonstrate persistent symptoms in a group of mildly infected, highly educated individuals.
Cognitive dysfunction and COVID-19
Recent studies have confirmed post-infectious cognitive dysfunction in survivors of COVID-19 (from ICU and ward hospitalization), and in non-hospitalized subjects3,9,10,60. However, cognitive impairment after mild infection (without hospitalization) is not well understood. In addition, it is not clear how hospitalization impacts neuropsychological functions, as literature is inconsistent in showing neuropsychological differences related to acute phase severity or hospitalization56,61,62. In a recent analysis of 35 patients after hospital discharge (12.6 years of education and approximately 26 days after discharge), the application of supervised neuropsychological tests revealed abnormal performances mainly in verbal fluency (11.4%), mental flexibility and working memory (8.6%)60. Our group of 74 non-hospitalized participants presented higher rates of impairments in phonemic verbal fluency (20.8%), semantic verbal fluency (16.3%), episodic immediate verbal memory (16.3%), and processing speed (11.7% in FDT-Reading and 10% in FDT-Counting). Compared with the above-mentioned study, we examine more participants and detected cognitive impairment, after a longer interval since the acute infection (approximately 79 days). So far, other researchers have applied a variety of non-supervised cognitive tests3,63 and also have demonstrated attention deficits in survivors. Despite the methodological differences (use of “web-optimized assessment”), one study63 evaluated a large sample of 81,337 individuals (although only 326 subjects had a confirmed COVID-19 diagnosis) and detected abnormalities in “higher cognitive or executive function”, especially in tasks with a semantic component, and in those requiring selective visual attention.
In a study64 that evaluated the cognitive functions of 740 patients (379 non-hospitalized; approximately 7.6 months after the COVID-19 infection), impairments were observed in processing speed attention, executive functions, phonological and semantic verbal fluency, and associated deficits in memory considering the coding and evocation steps. Interestingly, if we apply − 1.5 z-score as the criteria for impairment, we observe impaired phonemic verbal fluency in 16% of our group, which is comparable to the 11% reported. In addition, features of dysexecutive syndromes, including confusion and attentional difficulties, have been associated with cognitive complaints presented by patients after COVID-19 infection65. The online evaluation of a group of 18 young post-infected subjects (mean age 42 years) with median interval of 85 days after diagnosis detected alterations of short-term memory, attention and concentration66.
Guo et al.67 assessed cognitive deficits with online evaluation (including memory, language, and executive functions). The study compared 181 patients with self-reported COVID-19 (only 65 confirmed, combining mild, moderate and severe acute infections) with 185 healthy controls and reported poor memory performance when compared to the control group.
A systematic review and metanalysis10 analyzed 175 patients who recovered from COVID-19 and confirmed cognitive dysfunction compared to healthy controls. Despite the methodological differences (related to cognitive assessments, the inclusion of patients with severe acute infection and varied intervals after acute infection), which may have contributed to the moderate level of heterogeneity among studies (I2 = 63%), the sensitivity analysis yielded similar outcomes—suggesting the persistence of cognitive impairment, at least from 1 to 6 months.
Unfortunately, methodological variabilities (considering the inclusion criteria, interval after the diagnosis, and the severity of acute infection and assessment methods) among these cognitive studies compromise comparisons. However, regardless of these methodological differences (and variations in the interval after diagnosis), we also observed dysfunctions in language and executive functions, episodic memory, and processing speed that agree with the literature data. The fact that we detected cognitive impairment almost one year after the diagnosis for some individuals is not surprising, as one recent study confirmed the risk of cognitive dysfunction after 2 years9.
One intriguing fact is that we observed a high proportion of low average performance in our sample of patients (which has a high average level of education), including immediate and late verbal episodic memory, phonological and semantic verbal fluency, immediate visuospatial episodic memory, processing speed, and inhibitory control. Although most subjects did not present significant impaired scores compared with the normative data, we speculate that the low average performance affecting different domains may result in a negative impact in everyday life, especially in individuals with high levels of education and cognitive demands.
MRI analyses
DTI alterations
Although contradicting, some studies have demonstrated changes in WM in hospitalized survivors14,15,23,68. However, fewer investigated WM alterations in individuals after a mild infection16. While the evaluation of 22 hospitalized patients with 1-year follow-up showed lower FA in the corpus callosum of severe patients, another study with 60 hospitalized patients (3 months after discharge) observed higher FA associated with reduced MD, RD and AD14. Likewise, high fractional anisotropy was reported in the study of one individual with a post-COVID autoimmune encephalitis69. We recently evaluated 56 patients with mild-to-moderate acute infection (95% non-hospitalized, without assessment of symptoms of anxiety or depression)16 and did not identify significant alterations of FA, AD, RD and MD; however, there was a significant reduction of fiber density in different tracts, mostly in the left hemisphere. The analyses of 86 patients (29 hospitalized and 57 non-hospitalized; the average age of 50 years and approximately one year after the acute infection) compared to 36 controls identified an overall reduction of fractional anisotropy, mean diffusivity, axial diffusivity and radial diffusivity70. Contrary to our group of non-hospitalized subjects (without history or current neuropsychiatric symptoms), the authors included individuals with hospitalization (33%), symptoms of depression (27%; mean BDI-II of 14 points), anxiety (9%), and older age (mean age of 50 years). We raised the hypothesis that the reduction of DTI measurements in the study of Diez-Cirarda et al.70 (contrary to the elevated values of axial diffusivity in the present study) and the absence of changes in the study performed by Bispo et al.16 could be associated with the combination of different methodology and the clinical differences of the groups included in each study.
We considered the absence of past history or current presence of neuropsychiatric symptoms in our group of patients necessary to disentangle the interaction between symptoms of anxiety (and depression) and the COVID infection, considering the possible negative impact of both on the white matter structure. We had previously reported an association between intensity of anxiety symptoms and atrophy of orbitofrontal cortex13; another study of 42 patients (37 hospitalized) identified a negative correlation between BDI scores with AD in a small cluster in the left hemisphere23. Therefore, our present results suggest a specific impact of the SARS-CoV-2 in the white matter independent of mood changes. However, the significance and interpretation of higher values of AD in the absence of alterations of other diffusivities requires extreme caution, due to the complexity of biophysical properties of these metrics71. As we did not identify significant correlations between maps of AD and scores of fatigue, somnolence or cognitive tests, we speculate the possibility of a silent biological process driven by the infection (direct viral or immune activation) which we were unable to associate with any cerebral dysfunction. As increases of axial and radial diffusivities have been associated with aging in healthy adults72, the longitudinal analyses may elucidate if the increase of AD will persist and eventually reflect any accelerated aging of the white matter.
FC analyses
While some studies reported alterations of brain functional connectivity after acute COVID-1922,41,70,73,74, we did not identify differences of functional connectivity between groups of patients and controls. Nor did we observe correlations of Pcing connectivity with fatigue or somnolence. Fewer studies reported Default Mode Network alterations after COVID-1974,75. One group of researchers described higher intranetwork connectivity within the DMN and higher internetwork connectivity between the DMN and the Olfactory Network (13 controls and 22 subjects with olfactory dysfunction without information related to the severity of infection)74. Another study performed functional connectivity analysis (with whole brain, region-of-interest based technique) of a group with 45 subjects after COVID-19 (17 mild, 19 moderate, nine severe, without healthy controls) and reported a role of the Default Mode Network in neuropsychiatric alterations75.
Some reasons (other than the different methods applied to analyze functional connectivity)22,41,70,73,74 may explain the discrepancies between our negative findings and different patterns of alterations detected in the previous analyses. One major factor is the inconsistencies related to the definition of post-COVID syndrome, which has been heavily criticized recently26. Although some studies included patients after 3 to 6 months after acute infection41,73,76, one study evaluated hospitalized patients 2 weeks after the acute infection22. The severity of the initial infection is another critical factor for neuropsychological evaluation and neuroimaging analyses (as severe infection associated with long-term impaired cognition77,78 and cerebral atrophy, regardless the etiology29; however two studies exclusively evaluated hospitalized patients22,76, one did not specify74, and the other two studies (from the same group) compared patients with mild (21 subjects), moderate (20 subjects) and severe infection (9 subjects). Unfortunately, these last two studies41,73 only included a small group of mildly infected individuals (21 subjects) and did not include healthy controls to determine the true deviations from what would be considered as the normal pattern (compared to paired non-infected individuals). The presence of symptoms of anxiety and depression (which may affect functional connectivity regardless of the presence of systemic infection79 was not clearly described in most of the studies22,41,74. One study with 50 hospitalized patients demonstrated increased functional connectivity associated with severity of post-traumatic stress symptoms76, considering that these individuals also presented symptoms of anxiety and depression. Given all the differences between these previous reports and our group, we were not surprised with the absence of alterations of cerebral functional connectivity since our group of mildly infected patients did not present a history or current symptoms of anxiety (or depression), and was compared to a balanced group of non-infected individuals (who underwent the same stressful conditions of COVID pandemics).

Rachel Carter is a health and wellness expert dedicated to helping readers lead healthier lives. With a background in nutrition, she offers evidence-based advice on fitness, nutrition, and mental well-being.